Death From Childbirth and the Cincinnati Irish
By: Andrea Middendorf
One of the main causes for maternal deaths around the world for millennia has been complications from childbirth and only in very recent history has the mortality rate dropped significantly. In the late 1800s in Cincinnati, Ohio, it was still a great danger for many women. Some of the common complications from childbirth were a prolonged birth, excessive bleeding, and infection. A prolonged birth often meant that there were complications, such as a misshapen pelvis caused by the childhood illness rickets. Rickets occurs when bones become weak due to malnutrition or a Vitamin D deficiency. Another problem was excessive bleeding. In the 1800s, a post-partum hemorrhage was without adequate treatment and many women bled to death. In that era, most children were born at home with family and friends to help, though sometimes both midwives and doctors were involved in childbirth. Typically though, the doctor was only called when the birth was prolonged and death was a very real fear. Unfortunately, given that standard medical practices were not what they are now, oftentimes doctors brought with them the risk of infection. Even though Ignaz Philipp Semmelweis, a physician practicing at the General Hospital in Vienna, discovered in the mid-1800s that hand washing reduced the deadly puerperal fever, caused by a uterine infection following birth, he was largely rebuffed by many in the medical community. Additionally, for most doctors the training the received in obstetrics was basic and often noncompulsory. All in all, childbirth was a serious and dangerous business.
Research into the digitized Cincinnati birth and death records show this as well, and illustrate that death during childbirth could basically happen to anyone. A sample was collected of 62 women from the Cincinnati Area. On the death records, 17 listed additional, more specific causes of death than simply “childbirth.” Some include acute bronchitis, septicaemia[1], dropsy[2], infection of ovary, pelvic cellulitis[3], peritonitis[4], pneumonia, puerperal convulsions[5], rupture of uterus[6], uraimia[7], and a uterine hemorrhage[8]. Most women however, did not have any additional information about the cause of death beyond simply “childbirth.”
These women ranged in age from 16 to 54, with an average age of 31. This is interesting because in 1850, the average life expectancy for a white woman was 40.5, and in 1900 it was 51.08, meaning the average life expectancy was about 48 years old. This means that women who died in childbirth on average died 17 years before the average, while some died 32 years before, or six years after the average. While there was a wide range of ages, the majority of women in this sample who died during childbirth were between the ages of 26 and 30 (16 of the 62 women) and between 31 and 35 (18 of the 62 women). Moreover, almost every woman in this sample died before the average life expectancy of 48. The bar graph below illustrates this breakdown of age at time of death.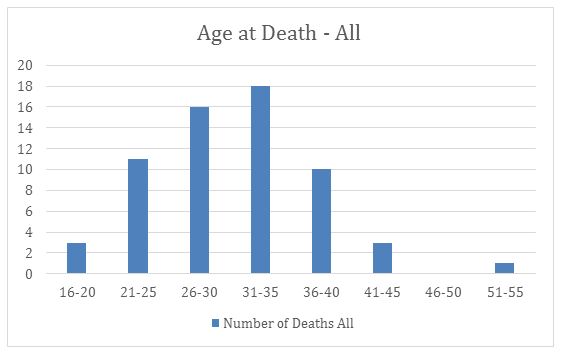
On the records, some listed the attending doctor who pronounced the death, the funeral home or undertaker, and the cemetery in which they are buried. The most frequently listed physicians were A.D. Stapleford, C.C. Agin, Carver, and Quinn. The most common funeral homes were Ackerman, Busse & Borgman, Dunkman, J. B. Habig, Lingers, Shreiber, Seelen, Sullivan, and Watkins. The most common cemeteries were Carthage Road, Raschig, Spring Grove, St. Joseph’s New, St. Mary’s, and Wesleyan. This is the information from all of the women whose information was collected. Included in this sample were women born in the United States and of English, German, Swiss, African, and Irish descent. 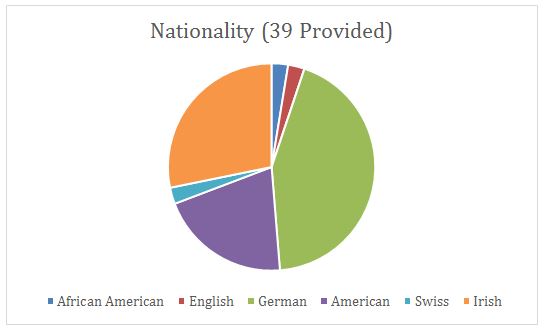
To focus on the Irish population in Cincinnati during this time, 11 of the 62 women sampled were Irish. Only one of these women, Elizabeth McCurdy, reported a specific complication: puerperal peritonitis. Compared with women who had not emigrated, giving birth was more dangerous in the United States than back in Ireland. At the turn of the 20th Century, the maternal mortality rate for Ireland was 618 per 100,000 births, whereas in the United States the rate was 850 per 100,000 births. When compared with the overall sample, the majority of the Irish-American women in Cincinnati also died in between the ages of 26 and 30 (4 of the 11 women) and between 31 and 35 (3 of the 11 women). The distribution is slightly more on the younger side than the sample as a whole though, as shown in this bar graph: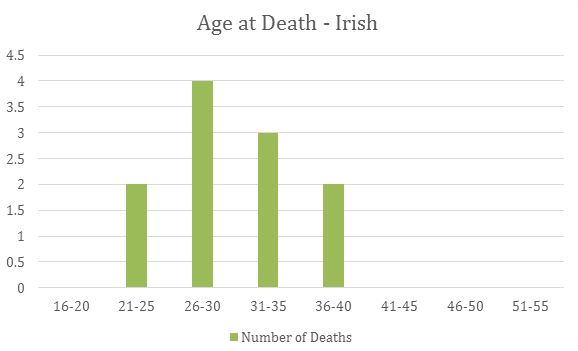
The doctors that were reported were Dunlap, Hazard, Richard, and Quinn; only Quinn was mentioned more than once. For funeral homes, Hackman, Lingers, and Miller were each mentioned once, and Sullivan was mentioned twice. It was reported that one woman was buried in Spring Grove, and four were buried in St. Joseph’s New (the rest were unreported). There were some very common names for these women: Margaret (three women), Julia (two women) and Elizabeth (two women). Interesting to note were the commonalities between two specific women: Ellen Coltigan and Bridget Marshall. Both died in the 31-35 age range, were pronounced dead by Dr. Quinn, had their funeral at Sullivan Funeral Home, and were buried at St. Joseph’s New. Both lived downtown, one on Broadway and one on Baymiller. They died eight years apart, one in 1870, and one in 1878.
Overall, childbirth was dangerous for all women at the time. However, through looking at the data, one can question whether was more dangerous for Irish-American women than it was for others, such as German-American women. Was there a significant socioeconomic difference between the German and Irish populations? And how might these differences been evident in other ethnic and racial populations such as Italians or African Americans? The Irish, for example, possibly may have been less likely than the Germans to have a doctor present during childbirth, as more than 50% of the Irish women did not have a doctor listed on their death card, while only about 23% of the overall population did not.
Bibliography
Davis, Rebecca. “The Doctor Who Championed Hand-Washing And Briefly Saved Lives.” NPR. NPR, 12 Jan. 2015. Web. 25 Mar. 2017. http://www.npr.org/sections/health-shots/2015/01/12/375663920/the-doctor-who-championed-hand-washing-and-saved-women-s-lives.
Department, Cincinnati (Ohio). Health. “Cincinnati Birth and Death Records, 1865-1912.” Digital Collections and Repositories @ UC Libraries. University of Cincinnati. Libraries, http://digital.libraries.uc.edu/collections/birthdeath/.
Ginnivan, Leah. “The Dirty History of Doctors’ Hands.” Method. Method, n.d. Web. 25 Mar. 2017. http://www.methodquarterly.com/2014/11/handwashing/.
“Life Expectancy by Age, 1850–2011.” Infoplease. Infoplease, n.d. Web. 21 Mar. 2017. http://www.infoplease.com/ipa/a0005140.html.
“Life Expectancy.” Wikipedia. Wikimedia Foundation, 23 Mar. 2017. Web. 25 Mar. 2017. https://en.wikipedia.org/wiki/Life_expectancy.
Roser, Max. “Maternal Mortality.” Our World In Data. N.p., n.d. Web. 21 Mar. 2017. https://ourworldindata.org/life-expectancy/.
[1] Septicaemia: When an abscess releases pus-forming bacteria into the bloodstream.
[2] Dropsy: When an excess of watery fluid collects in the cavities or tissues.
[3] Pelvic Cellulitis: When the parametrium (the tissue that separates the cervix from the bladder) gets a bacterial infection following childbirth.
[4] Peritonitis: When the peritoneum (the membrane lining the abdominal cavity and covering the abdominal organs) gets inflamed, typically due to a bacterial infection through the blood or following an abdominal organ’s rupture.
[5] Puerperal Convulsions: When a woman has spontaneous convulsions following childbirth.
[6] Rupture of Uterus: When the myometrial wall (part of the uterine wall) is breached. This can be an incomplete rupture where the peritoneum is still intact, or it could be a complete rupture where the uterus may spill into the peritoneal cavity.
[7] Uraimia: When the kidneys are unable to properly eliminate all of the urea and other nitrogenous waste out of the blood.
[8] Uterine Hemorrhage: When there is excessive bleeding postpartum.